Understanding Hypocalcemia: The Role of Calcium Lactate Gluconate in Managing Low Blood Calcium Levels
We all know calcium is crucial for strong bones and teeth, but its role extends far beyond that. This vital mineral is involved in muscle function, nerve transmission, blood clotting, and even hormone release. When calcium levels in the blood drop too low, a condition called hypocalcemia occurs. This blog post will delve into hypocalcemia, exploring its causes, symptoms, and traditional treatments, before focusing on the promising role of calcium lactate gluconate in managing this condition.
Brief overview of hypocalcemia
Hypocalcemia, simply put, is a condition characterized by abnormally low levels of calcium in the blood. It can range from mild and asymptomatic to severe and life-threatening.
Importance of calcium in the body
Calcium plays a multifaceted role in human physiology:
- Bone health: It’s the primary building block of bones and teeth, providing strength and structure [1].
- Muscle function: Calcium is essential for muscle contraction and relaxation.
- Nerve transmission: It facilitates communication between nerves.
- Blood clotting: Calcium is a key component in the coagulation cascade [2].
- Hormone release: It’s involved in the secretion of various hormones.
- Electrolyte imbalance: It is used to treat or prevent other electrolyte imbalances, such as hypokalemia (low potassium levels) or hypermagnesemia (high magnesium levels).
What is Hypocalcemia?
Definition and normal calcium levels
Hypocalcemia is defined as a total serum calcium level below 8.5 mg/dL (2.1 mmol/L). Normal calcium levels typically range from 8.5 to 10.5 mg/dL (2.1 to 2.6 mmol/L) [3]. It’s important to note that ionized calcium (the biologically active form) is often a more accurate measure, but total calcium is more commonly measured.
Common causes of low blood calcium levels
Several factors can contribute to hypocalcemia, including:
- Vitamin D deficiency: Vitamin D is crucial for calcium absorption.
- Hypoparathyroidism: Underactive parathyroid glands produce insufficient parathyroid hormone (PTH), which regulates calcium levels [4].
- Kidney disease: The kidneys play a vital role in calcium metabolism.
- Malabsorption: Conditions affecting nutrient absorption in the gut.
- Certain medications: Some drugs can interfere with calcium levels.
- Dietary deficiency: Inadequate calcium intake, although less common in developed countries.
Symptoms of low calcium levels in the blood
Symptoms can vary depending on the severity of hypocalcemia:
- Mild: Often asymptomatic.
- Moderate: Muscle cramps, spasms, tingling or numbness in the fingers, toes, or around the mouth [5].
- Severe: Tetany (muscle contractions), seizures, arrhythmias, and even heart failure.
Dietary recommendations for low blood calcium (hypocalcemia)
It focusses on increasing calcium intake through food sources. 1 Prioritize calcium-rich foods like dairy products (milk, yogurt, cheese), fortified plant-based milks, leafy green vegetables (kale, spinach, collard greens), tofu, fortified cereals and orange juice, and canned fish with edible bones (salmon, sardines). Consuming these foods regularly throughout the day, rather than in one large serving, can improve calcium absorption. It’s also important to ensure adequate vitamin D intake, as it plays a crucial role in calcium absorption. Sunlight exposure, fortified foods, and vitamin D supplements can help maintain sufficient levels. Limiting the intake of foods high in phytates (found in legumes and whole grains) and oxalates (found in spinach and rhubarb) can improve calcium bioavailability. If dietary intake is insufficient, calcium supplements may be necessary, but it’s essential to consult with a healthcare professional or registered dietitian to determine the appropriate dosage and type of supplement.
Traditional Treatments for Hypocalcemia
Overview of standard calcium supplements
Traditional treatments often involve oral calcium supplements like calcium carbonate or calcium citrate. Vitamin D supplementation is also crucial, especially in cases of deficiency.
Limitations and challenges in current treatments
Calcium carbonate requires stomach acid for absorption, making it less effective for individuals with low stomach acid (e.g., older adults or those taking certain medications) [6]. Calcium citrate has better absorption but may still have limitations. Furthermore, achieving and maintaining stable calcium levels can be challenging in some patients.
Introducing Calcium Lactate Gluconate: Best calcium supplements for hypocalcemia
Chemical composition and properties
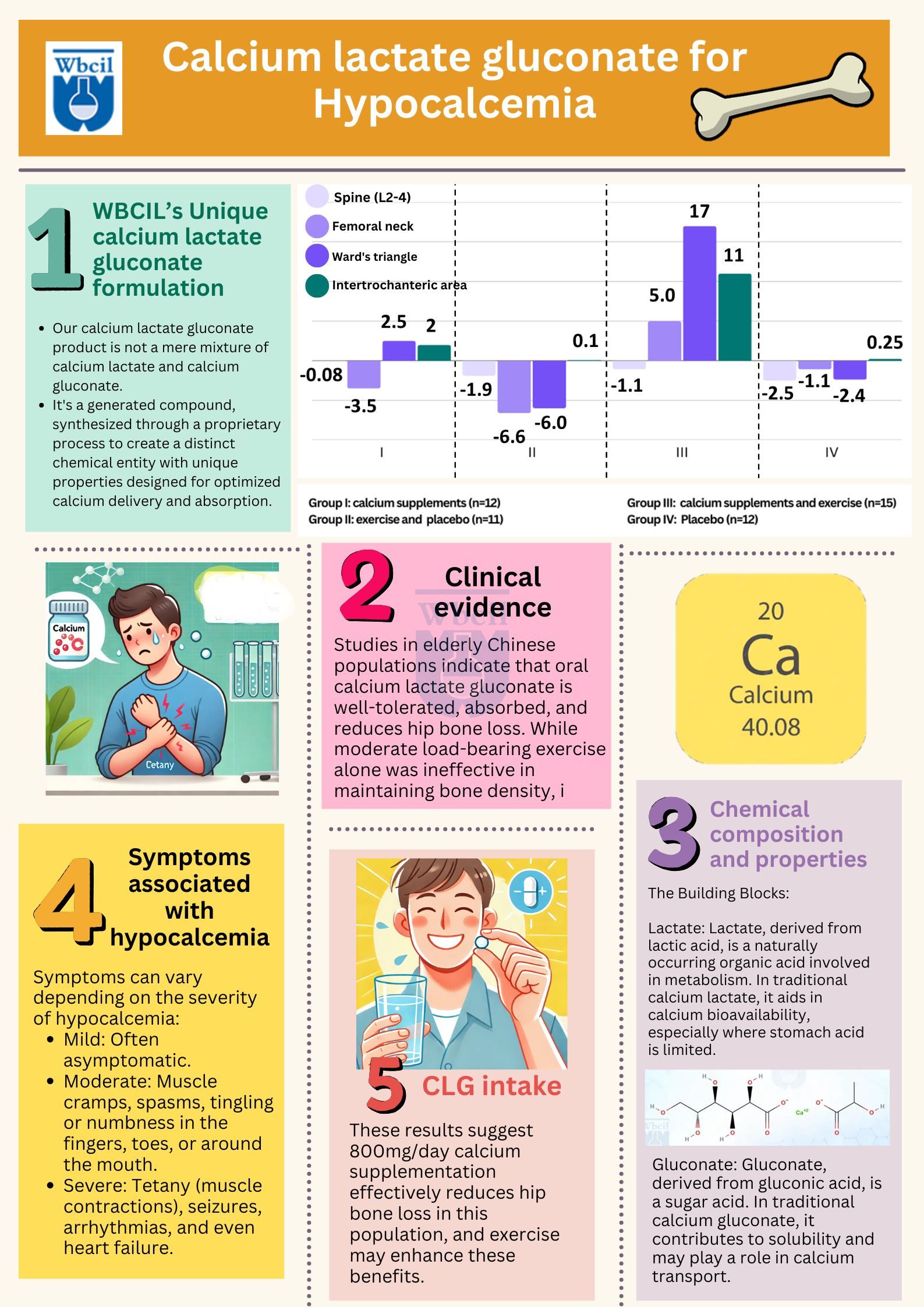
Our calcium lactate gluconate product is not a mere mixture of calcium lactate and calcium gluconate. It’s a generated compound, synthesized through a proprietary process to create a distinct chemical entity with unique properties designed for optimized calcium delivery and absorption [7]. This generated form offers potential advantages compared to simply combining the two salts. Understanding the properties of this novel compound is key to appreciating its therapeutic potential. Effective management of hypoglycemia in diabetes involves a multifaceted approach, including regular blood glucose monitoring, dietary adjustments, appropriate medication management, and prompt treatment of hypoglycemic episodes.
The Building Blocks: Understanding Lactate and Gluconate
While our product is a distinct compound, it’s helpful to understand the properties of the components from which it is derived:
- Lactate: Lactate, derived from lactic acid, is a naturally occurring organic acid involved in metabolism [8]. In traditional calcium lactate, it aids in calcium bioavailability, especially where stomach acid is limited.
- Gluconate: Gluconate, derived from gluconic acid, is a sugar acid. In traditional calcium gluconate, it contributes to solubility and may play a role in calcium transport [9].

Properties of the Generated Calcium Lactate Gluconate:
Our generated calcium lactate gluconate exhibits specific properties that make it advantageous for hypocalcemia management:
Comparison with other calcium supplements for low calcium in blood
Calcium lactate gluconate offers a potentially advantageous alternative to traditional calcium supplements, particularly for individuals with absorption issues.
Mechanism of Action: How Calcium Lactate Gluconate Works
Calcium Lactate Gluconate bioavailability and absorption
The combination of lactate and gluconate may enhance calcium absorption compared to calcium carbonate, even in individuals with reduced gastric acid [10].
Role in replenishing calcium levels in the blood
Calcium lactate gluconate provides a readily available source of calcium, helping to quickly replenish depleted levels in the blood [11].
Managing hypoglycemia in diabetes
Hypoglycemia in diabetes requires careful management. This includes regular blood glucose checks, consistent meals, and proper medication dosing. Recognizing and promptly treating low blood sugar symptoms with quick-acting carbohydrates is crucial. Working closely with healthcare providers is essential for personalized management.
Benefits of Using Pharmaceutical grade Calcium Lactate Gluconate in Hypocalcemia Management
Efficacy in correcting low calcium in blood levels
Studies suggest that calcium lactate gluconate can be effective in raising serum calcium levels.
Safety profile and tolerability
Generally well-tolerated, although some gastrointestinal side effects are possible.
Calcium Lactate Gluconate vs. other calcium supplements
Potentially improved absorption, especially in patients with low gastric acid or malabsorption issues.
Clinical Applications and Dosage Considerations
Recommended dosages for different patient populations
Dosage depends on the severity of hypocalcemia, the patient’s age, and other factors. Healthcare professionals determine the appropriate dose.
Potential side effects and contraindications
Possible side effects include nausea, vomiting, constipation, and diarrhea. Contraindications may include hypercalcemia (high calcium levels) or certain kidney conditions [12].
Monitoring and follow-up during treatment
Regular monitoring of serum calcium levels is crucial to ensure the effectiveness of treatment and prevent complications.
Case Studies and Research Findings
Studies in elderly Chinese populations indicate that oral calcium lactate gluconate is well-tolerated, absorbed, and reduces hip bone loss. While moderate load-bearing exercise alone was ineffective in maintaining bone density, it may synergistically interact with calcium supplements to reduce femoral neck bone loss. Given the low calcium intake typical in Hong Kong Chinese, investigating calcium’s impact on bone density is crucial. Similar to other studies, calcium supplementation prevented hip, but not spinal, bone loss in this elderly cohort, supporting a calcium threshold effect. Although exercise alone did not retard bone loss, possibly due to low calcium intake, its potential for improving muscle strength and fall prevention is important. These results suggest 800mg/day calcium supplementation effectively reduces hip bone loss in this population, and exercise may enhance these benefits.
Conclusion
Recap of key points
Hypocalcemia is a common condition with potentially serious consequences. Maintaining adequate calcium levels is essential for overall health.
Future perspectives in hypocalcemia treatment
Ongoing research continues to explore new and improved methods for managing hypocalcemia, including novel calcium compounds and drug delivery systems.
Encouragement for further research and consultation with healthcare professionals
If you suspect you may have hypocalcemia, it’s crucial to consult with a healthcare professional for diagnosis and treatment. Further research is encouraged to better understand and manage this condition. This information is for educational purposes only and should not be considered medical advice. Always consult with a qualified healthcare provider 1 for any health concerns or before making any decisions related to your health or treatment.
1. Wikipedia contributors. (2025, January 14). Calcium lactate gluconate. In Wikipedia, The Free Encyclopedia. Retrieved 11:09, February 13, 2025, from https://en.wikipedia.org/w/index.php?title=Calcium_lactate_gluconate&oldid=1269300284
2. https://go.drugbank.com/drugs/DB13365
3. National Center for Biotechnology Information (2025). PubChem Compound Summary for CID 91663257, Calcium lactate gluconate. Retrieved February 13, 2025 from https://pubchem.ncbi.nlm.nih.gov/compound/Calcium-lactate-gluconate.
4. Somasundaram, S., Jaya, T., Punnoose, A.M. et al. Fabrication and characterization of calcium lactate gluconate electrospun novel fibrous sheet for bone tissue engineering. emergent mater. 7, 2701–2710 (2024). https://doi.org/10.1007/s42247-024-00770-6
5. Phadungath, C., & Metzger, L. E. (2011). Effect of sodium gluconate on the solubility of calcium lactate. Journal of Dairy Science, 94(10), 4843–4849. doi:10.3168/jds.2011-4549. https://www.sciencedirect.com/science/article/pii/S0022030211005054
6. https://www.sciencedirect.com/science/article/abs/pii/S0920410522008476
7. https://www.webmd.com/drugs/2/drug-3709/calcium-lactate-oral/details
8. https://patents.google.com/patent/EP1516624A9/en
9. Choi JS, Kim JW, Kim KY, Cho HR, Choi IS, Ku SK. Antiosteoporotic effects of Polycan in combination with calcium lactate-gluconate in ovariectomized rats. Exp Ther Med. 2014 Sep;8(3):957-967. doi: 10.3892/etm.2014.1793. Epub 2014 Jun 20. PMID: 25120630; PMCID: PMC4113539. https://pmc.ncbi.nlm.nih.gov/articles/PMC4113539/
10. https://www.healthline.com/nutrition/calcium-lactate
11. https://www.ema.europa.eu/en/documents/referral/summary-information-referral-opinion-following-arbitration-pursuant-article-30-council-directive-200183ec-calcium-sandoz-and-associated-names-international-non-proprietary-name-inn-calcium-lactate_en.pdf
12. https://www.wikidoc.org/index.php/Calcium_lactate_gluconate
Hypocalcemia means low blood calcium. Calcium is vital for bones, muscles, and nerves. Low levels can cause various health problems. Hypocalcemia has many causes. Common ones include vitamin D deficiency, kidney disease, and certain medications. Parathyroid problems can also be a factor.
Low calcium symptoms vary. They may include muscle cramps, fatigue, and tingling. Severe cases can lead to seizures or heart problems.
A simple blood test diagnoses hypocalcemia. Doctors check your calcium level. Further tests may find the underlying cause.
Treatment depends on the cause and severity. It often involves calcium and vitamin D supplements. Doctors may also treat the underlying condition.
This is a calcium supplement. It helps raise calcium levels in the blood. It’s often used for mild to moderate hypocalcemia.
Side effects are usually mild. They can include stomach upset or constipation. Always follow your doctor’s dosage instructions.
Different calcium supplements exist. They vary in calcium content and absorption. Your doctor can recommend the best one for you.
Dosage depends on individual needs. Your doctor will prescribe the right amount. Never exceed the recommended dose.
Diet plays a key role. Eat calcium-rich foods like dairy and leafy greens. Fortified foods can also help.
See a doctor if you have symptoms. Early diagnosis and treatment are crucial. Don’t ignore potential signs of hypocalcemia.